“Effect of lung recruitment and titrated positive end-expiratory pressure (PEEP) vs low PEEP on mortality in patients with acute respiratory distress syndrome,” JAMA, 2017, Acute Respiratory Distress Syndrome Trial (ART) Investigators
Question: Do lung recruitment maneuvers paired with PEEP titrated to best respiratory system compliance improve outcomes for patients with moderate-severe ARDS?
Study Type: Multicenter randomized trial (120 ICUs in 9 countries)
Study Population: Mechanically ventilated patients with moderate-severe ARDS for <72 hours were eligible. Notable exclusion criteria included escalating doses of vasopressors, contraindications to hypercapnia (intracranial hypertension, ACS), and pneumothorax.
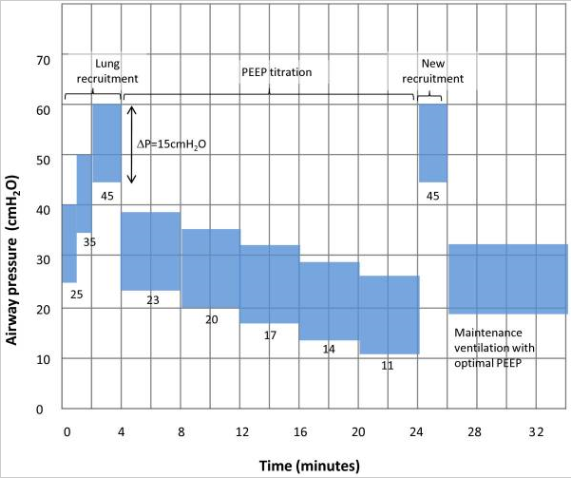
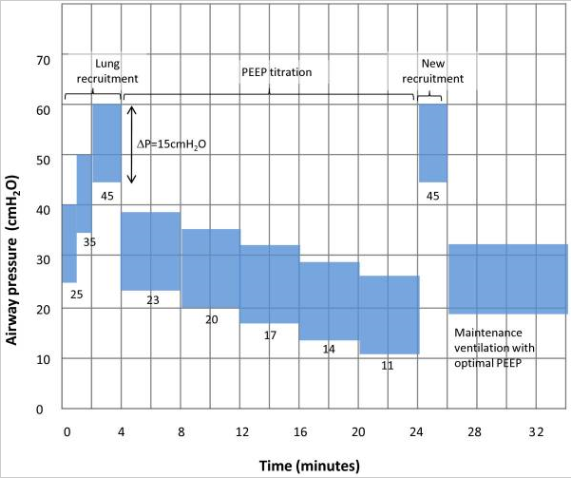
Study Groups: Patients in the control arm were managed per the ARMA/ARDSnet protocol (NEJM, 2000). Patients in the intervention arm received a bolus of a neuromuscular blocking agent followed by a recruitment maneuver with subsequent decremental PEEP titration (PEEP decreased by 3 cmH20 every 4 minutes until the highest respiratory system compliance was achieved). If P/F levels were stable or increasing for 24 hrs, PEEP was decreased by 2 cmH20 every 8 hrs. The initial recruitment maneuver utilized the following protocol: pressure control ventilation, Pi 15 cmH20, PEEP 25 cmH20 x 1 min, PEEP 35 cmH20 x 1 min, PEEP 45 cmH20 x 2 min (so breaths on the final step started at a PEEP of 45 cmH20 and increased to a Ppeak of 60 cmH20). After PEEP titration, the patients received a 2nd recruitment maneuver of PEEP 45 cmH20 x 2 minutes. After 556 pts, this protocol was modified after 3 patients in the intervention arm had a cardiac arrest possibly associated with the recruitment maneuver (!!). The revised protocol started at a PEEP of 25 cmH20 x 1 min then 30 cmH20 x 1 min then 35 cmH20 x 1 min with PEEP subsequently decreased in 3 minute intervals to find the highest compliance followed by a final recruitment maneuver of PEEP 35 cmH20 for 2 mins.
https://www.thebottomline.org.uk/summaries/icm/art/
Primary Outcome: 28-day mortality
Results: 1,010 patients were included in the final analysis. There were no notable differences between the two groups. 65% of patients had septic shock and 55% had pneumonia. The mean P/F was 119, both groups were receiving mean TVs of 5.8 mL/Kg IBW at enrollment, and 10% received prone positioning. At 28 days, 55.3% of pts in the intervention arm had died compared to 49.3% of pts in the control arm (HR 1.2 95% CI, 1.01-1.42; p=0.41). Patients in the intervention arm had significantly higher rates of death within 6 months, death within 7 days, pneumothorax requiring drainage within 7 days, and need for commencement or increase of vasopressors or hypotension within 1 hr. There were also 3 cases of cardiac arrest in the intervention arm.
Caveats: Study protocol changed in the middle of the study, multiple interventions used in experimental arm (more below)
Take-home Point: For patients with moderate-severe ARDS, a strategy that paired recruitment maneuvers with PEEP titrated to best respiratory system compliance was associated with harm compared to usual care.
Comments:
- Just so everyone is clear, for patients in the intervention arm, following the recruitment maneuver, the bedside clinician would switch the ventilator mode from AC-PC to AC-VC, drop PEEP from 45 cmH20 to 23 cmH20, wait 4 minutes, perform an inspiratory hold, and calculate compliance (Tv/Plt-PEEP). PEEP would then be decreased by 3 cmH20 and compliance again calculated after 4 minutes. This process was repeated until the PEEP with the highest compliance was identified. At this point, 2 cmH20 was added to that PEEP. The idea here is to “open up” as much of the lung as possible with the recruitment maneuver and then “keep it open” with some high level of PEEP that balances overdistension with de-recruitment.
- A major issue with interpreting this study is that the intervention arm actually includes multiple interventions (paralytics often paired with IVF, recruitment maneuvers, and a decremental PEEP trial). It is impossible to determine if one of those in particular contributed to the signal of harm in the trial (perhaps obscuring a signal of benefit from one of the other interventions) or if they acted synergistically.
- As in the ALVEOLI trial, higher levels of PEEP produced a physiologic benefit. Patients in the intervention arm had lower driving pressures, lower Pplts, and higher respiratory system compliance. So why didn’t this improve outcomes? The recruitment maneuvers were very aggressive, up to a PEEP of 45 cmH20 for 2 minutes until the protocol was changed after 3 cardiac arrests. Perhaps the signal of increased pneumothorax and barotrauma was because pts in the intervention arm were being subjected (often repeatedly) to very high airway pressures often combined with IVF which can worsen edema.
- As with the ALVEOLI trial pts in the control received exceptional care (far better than we do in practice) with a mean Tv <6 cc/kg IBW and Pplt <30. I think these trials show that when the ARMA (ARDSnet) protocol is followed, the additive survival benefit of any single additional vent maneuver is marginal. There is a lot of enthusiasm in the critical care community re: the use of driving pressure (Pplt – PEEP) to set PEEP and guide vent management. I think this trial should temper expectations that such a strategy will dramatically alter outcomes (despite a decrease in driving pressure, more patients in the intervention arm here died).
- The major PEEP trials are ALVEOLI (reviewed last time), ART (this trial), EXPRESS (JAMA, 2008), and LOVS (JAMA, 2008). All of them failed to show a signal of benefit in their primary outcome and one of the (ART) showed harm. Much has been written about benefits of higher PEEP in subgroups, PEEP responders (defined a bunch of different ways), and when data is pooled in meta-analyses. Those are all interesting but I think it’s really important to understand the major clinical trials, their limitations, and form your own conclusions to inform your practice.
See also:
The Bottom Line