Thanks to third-year Ale for hosting us at her rooftop patio!
Author Archives: Cathy
Proning practices before and after COVID
- Before COVID, proning was clearly underused
- Recommendation for proning by official ARDS guidelines are strong that severe ARDS should receive proning>12hr/day
- Anecdotally have seen more proning during COVID
- Full team is more comfortable and familiar with it – it’s less new, RT and nursing are used to it and ask about it, etc
- But what do the numbers show?
- Retrospective review of proning during COVID 2020-2021 or pre-COVID ARDS 2018-2019 at academic and community hospitals
- Proning initiated faster and more in COVID vs historic ARDS (58%!!! vs 9%)
- Practice sustained throughout the pandemic
- Time will show if things will change over time if COVID numbers continue to stay low
Morning Report 6/28 – Chylothorax
Some highlights about chylothorax from Amy’s great morning report case.

Chylothorax (picture from StatPearls:https://www.ncbi.nlm.nih.gov/books/NBK459206/)
- Equal incidence of traumatic (during surgery in chest) vs non-traumatic (malignancy causing compression or lymphoma, also lots of idiopathic/misc causes)
- Gold standard: chylomicrons in fluid – lipoprotein electrophoresis but this is often not available
- Cutoff: using triglycerides as surrogate, TG>110 mg/dL very likely chylothorax, TG<50 very unlikely to be chylothorax
- Gross appearance of fluid not that sensitive for diagnosis, less than half of cases have the classic milky appearance
- IR lymphagiogram – injecting lipophilic contrast agent into a lymph node and watching it ascend into the abdomen to identify the cisterna chyli
- Recommendations: special diet ultra-low in middle chain fatty acids (<10g per day, aka less than one piece of pizza, 3 pieces of bacon, and dove chocolate bar) – decreased chylomicrons > decreased chyle
- Other options include thoracic duct embolization, ligation (especially for high-volume chyle leak from thoracic duct injury), pleurodesis, pleuroperitoneal shunt, octreotide, somastatin etc
Sources:
Amy Ludwig’s Morning Report
Congratulations to the PCCM Fellowship Class of 2022!

Congratulations to the PCCM Fellowship Class of 2022!





Thanks to Justin Fiala for these awesome 3D printed lung planters!

Hand-washing and C.diff contact precautions
I tried to find data on alcohol based hand rubs in C.diff but all I found is that hand washing is recommended – see this small study of volunteers who had C.diff spores spread on their hands then either soap or alcohol, then shook hands with other volunteers – hand washing was better at removing spore counts – https://pubmed.ncbi.nlm.nih.gov/20429659
Surprisingly, the IDSA guidelines – https://www.idsociety.org/practice-guideline/clostridium-difficile/– say okay to do alcohol based cleaning if gloves are worn in routine and non-endemic settings, though acknowledges that handwashing with soap and water is superior to alcohol based hand hygiene
My practice will be to continue hand-washing after C.diff rooms, time-consuming as it is, because don’t want to bring it home to your cat or dog (happened to one of my residents; https://www.hcplive.com/view/potential-transfer-of-clostridium-difficile-from-dog-cat-to-household-owners)
CCR22!
Lots of activity on Twitter on CCR22 during the current Critical Care Review Meeting – #CCR22
Blood biofire?
I read a little more about the blood culture biofire that we’ve started seeing – BCID2 – 43 PCR results including organisms and resistance – https://www.biofiredx.com/products/the-filmarray-panels/filmarraybcid/ and some evidence – Banerjee et al randomized 617 patients with positive blood cultures to usual care (takes about two days to get results from micro lab cultures) vs BCID +- stewardship team – showed shorter time to organism identification and appropriate abx changes – no difference in mortality, LOS, or cost
![Comparison of time to organism identification, availability of phenotypic antimicrobial susceptibility results, and first appropriate modification of antimicrobial therapy for the subset of study subjects with organisms represented on the rapid multiplex polymerase chain reaction (rmPCR) panel (n = 481). Time 0 is when the positive Gram stain result was reported. Median time in hours (interquartile range [IQR]) to organism identification: control 22.3 (17–28), both rmPCR and rmPCR + stewardship 1.3 (0.9–1.6); de-escalation: control 39 (19–56), rmPCR 36 (22–61), rmPCR + stewardship 20 (6–36); escalation: control 18 (2–63), rmPCR 4 (1.5–24), rmPCR + stewardship 4 (1.8–9). *P < .05 vs control; †P < .05 vs control and rmPCR groups.](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/cid/61/7/10.1093_cid_civ447/1/m_civ44702.gif?Expires=1656615705&Signature=uh-Nv-ujh61U-Py8oZJa68o69fm10gzyNUYaLXd1MxR0febizhFFF97Xh0gMd3mJ3O-blQAJWKhQ~homJFlHMDgT~hft2KzOz1qmWvBDIsLg3LHtNh8pFE~zJ3vm6~lztWgAu3ixAcmqWV-esiEevvNG3glObWz2LXRXmV-4X3qSSySR-1VdqvVXpHkxeaOgN1v0N8Sm0KKqnHb65ifX8yK5UxYVmmrkSNdbyzWyi4IgLmAiulXeu5Xdvtq6jK3wbwsd2E0AD5wIQbUNkAc7Xf-s6fZ9P5iMdguVOFYPVyWaLL5kWPsLadiQEUEs2KmrerbW6nOd~Ofvbx38C4mDmg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA) https://academic.oup.com/cid/article/61/7/1071/289120 They also have a small number of discrepancies (11 cases) in their Table 2 – but pretty reasonable and only 3 true cases of organism identification discrepancy
https://academic.oup.com/cid/article/61/7/1071/289120 They also have a small number of discrepancies (11 cases) in their Table 2 – but pretty reasonable and only 3 true cases of organism identification discrepancy
I’m excited to see this and look forward to using it clinically!
Iron and the ICU
Iron is needed by bacteria
Higher iron associated with higher mortality in ICU patients – https://www.nature.com/articles/s41598-018-29353-2
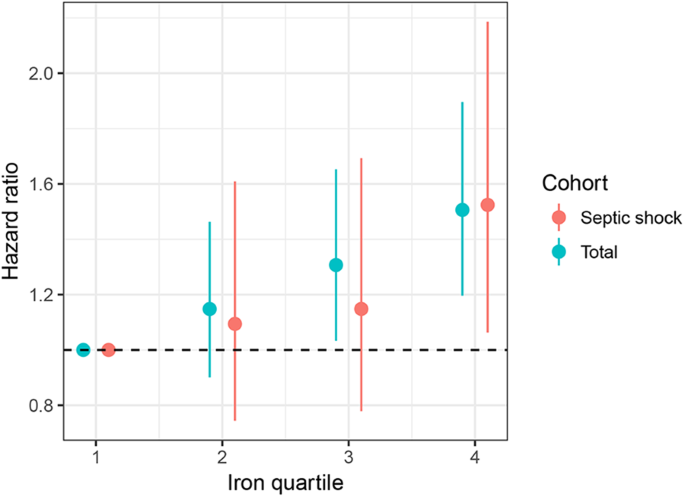
Animal sepsis models – giving iron in septic animals leads to increased mortality – https://pubmed.ncbi.nlm.nih.gov/15190970/
Giving IV iron to stable outpatients doesn’t necessarily increase infections – https://pubmed.ncbi.nlm.nih.gov/31485910/
But wouldn’t give it to septic patients (though note the data for this are sparse – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3226152/)
 In fact, check out Cefiderocol – trojan horse antibiotic – two cephalosporins (ceftaz, cefepime) and catechol-type siderophore ~iron – gets taken up by bacteria but then attacked by antimicrobial! – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7054475/ – just recently approved
In fact, check out Cefiderocol – trojan horse antibiotic – two cephalosporins (ceftaz, cefepime) and catechol-type siderophore ~iron – gets taken up by bacteria but then attacked by antimicrobial! – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7054475/ – just recently approved

DEXA-ARDS – steroids for ARDS?
DEXA-ARDS study – Villar et al. in Lancet Resp –
https://www.thelancet.com/pdfs/journals/lanres/PIIS2213-2600(19)30417-5.pdf
https://www.thelancet.com/pdfs/journals/lanres/PIIS2213-2600(19)30417-5.pdf
RCT of 277 patients with ARDS P/F<200 todexa 20 daily x 5d then down to 10mg x5d or extubation; improved outcomes vent-free days, mortality (21% vs 36% at 60 days)! Rich says every few years steroids for ARDS come back into vogue but then another study shows no benefit or harm and the cyclerepeats though.

Pulmcrit has a nice summary of the previous studies too of steroids in ARDS – https://emcrit.org/pulmcrit/dexa-ards/
High-Impact PCCM article summaries: Ultrasound Assessment of JVP to Predict Elevated RAP
Wang et al. Accuracy of Ultrasound Jugular Venous Pressure Height in Predicting Central Venous Congestion. Annals of Internal Medicine. 2022
Question: Does ultrasound assessment of jugular venous pressure height (uJVP) in the semi-upright and upright positions predict elevated right atrial pressure (RAP) measured during right heart catheterization (RHC)?
Why ask it: Visual inspection of the height of the JVP is often used to estimate RAP. Patient anatomy and variation in the distance between the sternal angle and right atrium may limit the accuracy of this measurement. While ultrasound assessment of inferior vena cava (IVC) diameter and collapsibility is commonly used to estimate RAP, there are many patient and operator-specific limitations to this technique.
Intervention: Convenience sample of 100 patients undergoing RHC at the University of Utah. Two POCUS-trained cardiology fellows and 1 attending physician obtained the following values using a handheld ultrasound (Butterfly Network):
1. Quantitative uJVP: measured with HOB at 30-45° and defined as the point at which the internal jugular (IJ) vein tapered to smaller than the adjacent carotid artery throughout the respiratory cycle (vertical height of this taper above sternal angle + 5 cm = uJVP).
2. Qualitative uJVP based on neck zone where the IJ collapse point was identified: zone 1 (below clavicle), zone 2 (lower 3rd of neck), zone 3 (middle 3rd of neck), zone 4 (upper 3rd of neck), and zone 5 (above mandible).
3. Qualitative uJVP with HOB 90°: If IJ distended to at least the size of the adjacent carotid artery, this test was considered positive
Results:
- ROC of uJVP as a continuous variable to predict RAP > 10 mmHg:
- AUC 0.84 (95% CI, 0.76 – 0.92)
- Test characteristics of uJVP > 8 cm to predict RAP > 10 mmHg:
- Sensitivity: 72.7% (95% CI, 57.2% – 85.0%), Specificity: 78.6% (95% CI, 65.5% – 88.4%), likelihood ratio: 3.4 (95% CI, 2.0 – 5.8)
- Test characteristics of qualitative uJVP with HOB 90° to predict RAP > 10 mmHg:
- Sensitivity 54.5% (95% CI, 38.8% – 69.6%), Specificity: 94.6% (85.1% – 98.9%)
- Evaluating correlation between 5 neck zones and uJVP showed a linear relationship with increasing RAP (figure pasted below)
Conclusion: Point-of-care ultrasound assessment of JVP can identify patients with an elevated RAP on RHC with a reasonable degree of accuracy
Comment:
- Important to emphasize this study looked at the relationship between JVP and RAP, not JVP and fluid responsiveness (i.e., will this patient increase their stroke volume in response to a fluid challenge). Two very different questions.
- Study cohort:
- LVEF < 50%: 44%
- Male: 64%
- White: 76%
- Presenting for evaluation of heart failure: 67%
- Outpatients: 40%
- Mean RAP: 10.3 mmHg
- Mean PCWP: 17 mmHh
- Limitations: Single-center study, convenience sample of 100 patients out of a potential 4,436 patients presenting for RHC during study period (possible selection bias), largely white and male population, not necessarily representative of MICU population, unclear generalizability of study findings to less experienced ultrasonographers
- Visual assessment of JVP had similar test characteristics to uJVP (supporting use of traditional method of JVP assessment for those who like this technique). However, uJVP was possible in 100% of patients while visual estimation was possible in only 60% of assessed patients.
- I like this study because it asks a simple question and gives helpful test characteristics to inform an individual clinician’s decision on whether to incorporate this technique into their clinical practice.
- All measured values in the ICU (e.g., Pplt, Pes, P0.1, CVP, PCWP, IVC collapsibility index, PPV, etc) are imperfect surrogates for complex physiology. In my view, the utility of any of these tests depends on the clinical question being asked, a clinician’s awareness of a specific test’s characteristics and limitations, and how thoughtfully a given value is combined with other data. Based on this study, if your clinical question is,“does my patient have an elevated RAP?,” ultrasound assessment of the IJ may be helpful.
- My take-home: I have always liked scanning the IJ (seems like a logical extension of scanning the heart and IVC + our MICU population seems enriched for patients in whom visual assessment of JVP is challenging). I prefer qualitative “big picture” patterns over quantitative bedside assessments as I worry about accuracy and over-interpretation with the latter. What I will consider using in practice:
- Seeing a zone 4 or 5 uJVP seems to be a reasonable surrogate for a RAP > 10 mmHg
- Visualization of the uJVP with the patient at 90° (not feasible in some MICU pts) has a high specificity for a RAP > 10 mmHg







