Thanks to David Kidd for presenting a cool IP case:




A nice resource provided by Tim:

Naranje, P., & Das, A. (2018). Approach to Airway Infections. Clinico Radiological Series: Imaging of Chest Infections, 418.
Thanks, David!

David Kidd, MD, Medicine
Thanks to David Kidd for presenting a cool IP case:




A nice resource provided by Tim:

Naranje, P., & Das, A. (2018). Approach to Airway Infections. Clinico Radiological Series: Imaging of Chest Infections, 418.
Thanks, David!

David Kidd, MD, Medicine
Question: Is high-flow nasal cannula non-inferior to non-invasive ventilation (NIV) in reducing rates of reintubation and postextubation respiratory failure in high risk patients?
Study Type: Multicenter, randomized, non-inferiority trial in 3 ICUs in Spain
Study Population: Patients receiving mechanical ventilation > 12 hours were eligible for the trial if they met at least one of the following criteria: age >65, CHF as primary indication for MV, mod-severe COPD, APACHE II >12 on day of extubation, BMI >30, airway patency problems, inability to deal with respiratory secretions, difficult weaning, 2 or more co-morbidities, or MV > 7 days. Exclusions included DNR, tracheostomies, and self-extubations.
Study Groups: Patients in the HFNC arm were placed on HFNC with flow set at 10L/min which was titrated up at 5L/min intervals until pts experienced discomfort. FIO2 was titrated to keep SpO2 > 92%. Patients in the NIV arm had PEEP and IPAP adjusted to targets of RR 25, SaO2 92, and pH 7.35. FiO2 was titrated to an SpO2 of at least 92%. Both groups were switched to conventional O2 after 24 hrs.
Primary Outcomes: Reintubation and postextubation respiratory failure within 72 hrs. Non-inferiority margin set at 10%

Results: 604 patients were randomized. Notable patient characteristics: respiratory failure as primary diagnosis (56%), surgical patients (38%), neurology patients (3%), median # of high risk factors (3). HNFC was non-inferior to NIV (19.1% of pts required reintubation in NIV group vs 22.8% in HFNC group). More patients in the NIV group experienced postextubation respiratory failure (26.9% HFNC vs 39.8% NIV). Close to 50% of NIV patients were unable to tolerate therapy for the full 24 hours (median duration 14 hrs). Other than a small reduction in ICU LOS with HFNC, secondary outcomes were similar between the two groups.
Caveats: Both HFNC and NIV were given for only 24hrs (in contrast to some other studies with longer periods of therapy), sedatives to facilitate NIV tolerance were not allowed, trial was not blinded.
Take-home Point: In high risk patients, HFNC appears non inferior to NIV in reducing rates of reintubation and postextubation respiratory failure.
In her morning report case last Wednesday, first year fellow Emily Olson focused on a case of secondary spontaneous pneumothorax (SSP) with delayed resolution. Remember, think about IP/thoracic surgery involvement if you’ve got leak for a week (or 5 days)

One strategy for managing persistent pneumothorax is endobronchial valve use. Because most of us are familiar with use of valves in COPD lung volume reduction, we reviewed the inclusion/exclusion criteria for use in this context (LIBERATE trial, AJRCCM 2018)

While noting that these criteria do not apply to application of valves for persistent pneumothorax

Finally, we discussed 2 methods used to guide endobronchial valve deployment for persistent air leak:

Source: Respiratory Medicine 137 (2018) 213–218
Great discussion, Emily!

Callback to this post, “Alpha-1 antitrypsin (AAT) deficiency, by PD Clara Schroedl”
Kaitlyn (@KaitlynVitale) reviewed the case of a middle-aged woman with severe pulmonary hypertension.
Shunt run and shunt ratio – reminder that these are samples taken during a right heart cath and can be used to calculate a ratio (nice review in PCIpedia)
Hereditary Hemorrhagic Telangiectasia – HHT
Rare 1:5000-8000 autosomal dominance (ENG, ACVRL2, SMAD4) – vascular AVMs (nosebleeds, GI bleeds, liver AVMs)



Discussion included the importance of genetic testing to predict outcomes (saliva kit for HHT panel), what classification this should fall under (group 3 high output heart failure vs group 5).

Great case, Kaitlyn!

Question: Do lung recruitment maneuvers paired with PEEP titrated to best respiratory system compliance improve outcomes for patients with moderate-severe ARDS?
Study Type: Multicenter randomized trial (120 ICUs in 9 countries)
Study Population: Mechanically ventilated patients with moderate-severe ARDS for <72 hours were eligible. Notable exclusion criteria included escalating doses of vasopressors, contraindications to hypercapnia (intracranial hypertension, ACS), and pneumothorax.
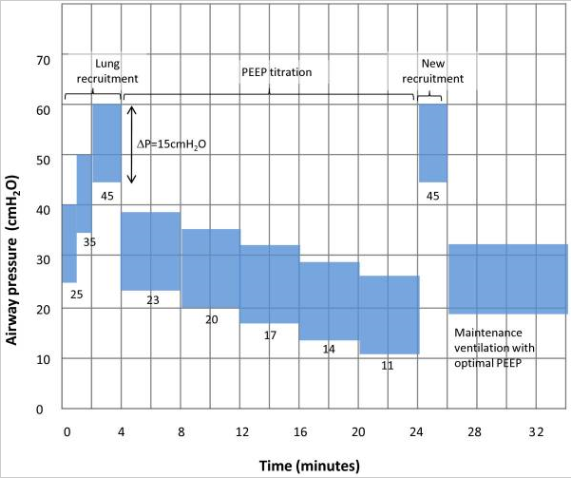
Study Groups: Patients in the control arm were managed per the ARMA/ARDSnet protocol (NEJM, 2000). Patients in the intervention arm received a bolus of a neuromuscular blocking agent followed by a recruitment maneuver with subsequent decremental PEEP titration (PEEP decreased by 3 cmH20 every 4 minutes until the highest respiratory system compliance was achieved). If P/F levels were stable or increasing for 24 hrs, PEEP was decreased by 2 cmH20 every 8 hrs. The initial recruitment maneuver utilized the following protocol: pressure control ventilation, Pi 15 cmH20, PEEP 25 cmH20 x 1 min, PEEP 35 cmH20 x 1 min, PEEP 45 cmH20 x 2 min (so breaths on the final step started at a PEEP of 45 cmH20 and increased to a Ppeak of 60 cmH20). After PEEP titration, the patients received a 2nd recruitment maneuver of PEEP 45 cmH20 x 2 minutes. After 556 pts, this protocol was modified after 3 patients in the intervention arm had a cardiac arrest possibly associated with the recruitment maneuver (!!). The revised protocol started at a PEEP of 25 cmH20 x 1 min then 30 cmH20 x 1 min then 35 cmH20 x 1 min with PEEP subsequently decreased in 3 minute intervals to find the highest compliance followed by a final recruitment maneuver of PEEP 35 cmH20 for 2 mins.
https://www.thebottomline.org.uk/summaries/icm/art/
Primary Outcome: 28-day mortality
Results: 1,010 patients were included in the final analysis. There were no notable differences between the two groups. 65% of patients had septic shock and 55% had pneumonia. The mean P/F was 119, both groups were receiving mean TVs of 5.8 mL/Kg IBW at enrollment, and 10% received prone positioning. At 28 days, 55.3% of pts in the intervention arm had died compared to 49.3% of pts in the control arm (HR 1.2 95% CI, 1.01-1.42; p=0.41). Patients in the intervention arm had significantly higher rates of death within 6 months, death within 7 days, pneumothorax requiring drainage within 7 days, and need for commencement or increase of vasopressors or hypotension within 1 hr. There were also 3 cases of cardiac arrest in the intervention arm.
Caveats: Study protocol changed in the middle of the study, multiple interventions used in experimental arm (more below)
Take-home Point: For patients with moderate-severe ARDS, a strategy that paired recruitment maneuvers with PEEP titrated to best respiratory system compliance was associated with harm compared to usual care.
Comments:
See also:
Wednesday’s Morning Report featured first year Emily Olson (@EmilyOlsonMD) leading a discussion of cavitary lung disease. Let’s review some of her learning points together!
First off, how much better of a mnemonic can you get for cavitary lung diseases than “CAVITY”?

It’s always helpful to look at previous chest imaging, and this is especially true in cavitary lung diseases! An important early diagnostic branch point is chronicity of process (12 weeks as the cutoff for a chronic process)

Histoplasmosis is one differential consideration for subacute/chronic cavitary lung disease which we commonly test for non-invasively.
We learned that the performance characteristics of testing depends on stage of disease.

Thanks for leading a great discussion, Emily!
 Sources cited
Sources cited
Today’s Morning Report featured a case of restrictive lung disease related to diffuse pleural thickening. Below are some of the points I hope you take away from the discussion:
I. Differential diagnosis of diffuse pleural thickening (DPT)
History is essential for differential diagnosis. 2 general categories:
II. Timeline of asbestos-related pulmonary disease

Legend – BAPE (Benign Asbestos-related Pleural Effusion), DPT (Diffuse Pleural Thickening) Clockwise from top left: DPT, pleural plaques, mesothelioma, ILD/asbestosis, BAPE
Remember that timeline is fluid, not absolute!
III. 3 distinct benign responses to asbestos exposure

Asbestos plaques involve parietal pleura only – lung sliding remains intact

Asbestosis – pulmonary fibrosis does not involve the pleura; septal thickening, reticulations (left) & honeycombing (center) are observed.

Diffuse pleural thickening involves inflammation at the visceral pleural border. Several findings associated with this, clockwise from top left; parenchymal bands “crow’s feet” associated with volume loss, a prominent parenchymal band, rounded atelectasis
IV. PET-CT may have utility in diagnostic evaluation of pleural thickening

Sources cited: