Wang et al. Accuracy of Ultrasound Jugular Venous Pressure Height in Predicting Central Venous Congestion. Annals of Internal Medicine. 2022
Question: Does ultrasound assessment of jugular venous pressure height (uJVP) in the semi-upright and upright positions predict elevated right atrial pressure (RAP) measured during right heart catheterization (RHC)?
Why ask it: Visual inspection of the height of the JVP is often used to estimate RAP. Patient anatomy and variation in the distance between the sternal angle and right atrium may limit the accuracy of this measurement. While ultrasound assessment of inferior vena cava (IVC) diameter and collapsibility is commonly used to estimate RAP, there are many patient and operator-specific limitations to this technique.
Intervention: Convenience sample of 100 patients undergoing RHC at the University of Utah. Two POCUS-trained cardiology fellows and 1 attending physician obtained the following values using a handheld ultrasound (Butterfly Network):
1. Quantitative uJVP: measured with HOB at 30-45° and defined as the point at which the internal jugular (IJ) vein tapered to smaller than the adjacent carotid artery throughout the respiratory cycle (vertical height of this taper above sternal angle + 5 cm = uJVP).
2. Qualitative uJVP based on neck zone where the IJ collapse point was identified: zone 1 (below clavicle), zone 2 (lower 3rd of neck), zone 3 (middle 3rd of neck), zone 4 (upper 3rd of neck), and zone 5 (above mandible).
3. Qualitative uJVP with HOB 90°: If IJ distended to at least the size of the adjacent carotid artery, this test was considered positive
Results:
- ROC of uJVP as a continuous variable to predict RAP > 10 mmHg:
- AUC 0.84 (95% CI, 0.76 – 0.92)
- Test characteristics of uJVP > 8 cm to predict RAP > 10 mmHg:
- Sensitivity: 72.7% (95% CI, 57.2% – 85.0%), Specificity: 78.6% (95% CI, 65.5% – 88.4%), likelihood ratio: 3.4 (95% CI, 2.0 – 5.8)
- Test characteristics of qualitative uJVP with HOB 90° to predict RAP > 10 mmHg:
- Sensitivity 54.5% (95% CI, 38.8% – 69.6%), Specificity: 94.6% (85.1% – 98.9%)
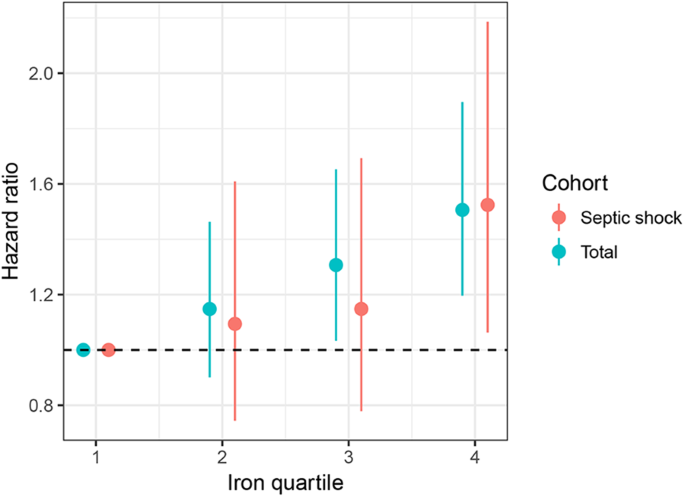
- Evaluating correlation between 5 neck zones and uJVP showed a linear relationship with increasing RAP (figure pasted below)
Conclusion: Point-of-care ultrasound assessment of JVP can identify patients with an elevated RAP on RHC with a reasonable degree of accuracy
Comment:
- Important to emphasize this study looked at the relationship between JVP and RAP, not JVP and fluid responsiveness (i.e., will this patient increase their stroke volume in response to a fluid challenge). Two very different questions.
- Study cohort:
- LVEF < 50%: 44%
- Male: 64%
- White: 76%
- Presenting for evaluation of heart failure: 67%
- Outpatients: 40%
- Mean RAP: 10.3 mmHg
- Mean PCWP: 17 mmHh
- Limitations: Single-center study, convenience sample of 100 patients out of a potential 4,436 patients presenting for RHC during study period (possible selection bias), largely white and male population, not necessarily representative of MICU population, unclear generalizability of study findings to less experienced ultrasonographers
- Visual assessment of JVP had similar test characteristics to uJVP (supporting use of traditional method of JVP assessment for those who like this technique). However, uJVP was possible in 100% of patients while visual estimation was possible in only 60% of assessed patients.
- I like this study because it asks a simple question and gives helpful test characteristics to inform an individual clinician’s decision on whether to incorporate this technique into their clinical practice.
- All measured values in the ICU (e.g., Pplt, Pes, P0.1, CVP, PCWP, IVC collapsibility index, PPV, etc) are imperfect surrogates for complex physiology. In my view, the utility of any of these tests depends on the clinical question being asked, a clinician’s awareness of a specific test’s characteristics and limitations, and how thoughtfully a given value is combined with other data. Based on this study, if your clinical question is,“does my patient have an elevated RAP?,” ultrasound assessment of the IJ may be helpful.
- My take-home: I have always liked scanning the IJ (seems like a logical extension of scanning the heart and IVC + our MICU population seems enriched for patients in whom visual assessment of JVP is challenging). I prefer qualitative “big picture” patterns over quantitative bedside assessments as I worry about accuracy and over-interpretation with the latter. What I will consider using in practice:
- Seeing a zone 4 or 5 uJVP seems to be a reasonable surrogate for a RAP > 10 mmHg
- Visualization of the uJVP with the patient at 90° (not feasible in some MICU pts) has a high specificity for a RAP > 10 mmHg















![Comparison of time to organism identification, availability of phenotypic antimicrobial susceptibility results, and first appropriate modification of antimicrobial therapy for the subset of study subjects with organisms represented on the rapid multiplex polymerase chain reaction (rmPCR) panel (n = 481). Time 0 is when the positive Gram stain result was reported. Median time in hours (interquartile range [IQR]) to organism identification: control 22.3 (17–28), both rmPCR and rmPCR + stewardship 1.3 (0.9–1.6); de-escalation: control 39 (19–56), rmPCR 36 (22–61), rmPCR + stewardship 20 (6–36); escalation: control 18 (2–63), rmPCR 4 (1.5–24), rmPCR + stewardship 4 (1.8–9). *P < .05 vs control; †P < .05 vs control and rmPCR groups.](https://oup.silverchair-cdn.com/oup/backfile/Content_public/Journal/cid/61/7/10.1093_cid_civ447/1/m_civ44702.gif?Expires=1656615705&Signature=uh-Nv-ujh61U-Py8oZJa68o69fm10gzyNUYaLXd1MxR0febizhFFF97Xh0gMd3mJ3O-blQAJWKhQ~homJFlHMDgT~hft2KzOz1qmWvBDIsLg3LHtNh8pFE~zJ3vm6~lztWgAu3ixAcmqWV-esiEevvNG3glObWz2LXRXmV-4X3qSSySR-1VdqvVXpHkxeaOgN1v0N8Sm0KKqnHb65ifX8yK5UxYVmmrkSNdbyzWyi4IgLmAiulXeu5Xdvtq6jK3wbwsd2E0AD5wIQbUNkAc7Xf-s6fZ9P5iMdguVOFYPVyWaLL5kWPsLadiQEUEs2KmrerbW6nOd~Ofvbx38C4mDmg__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)
 In fact, check out
In fact, check out 


