By Rebecca Wurtz
 Bench science and public health are two concepts that don’t often appear in the same sentence. Practitioners of each have a different world view, literally and figuratively. When we picture a bench scientist, we imagine someone peering through a microscope, focused on the most minute components of health and disease. When we think of public health, we picture someone who sees the world as a series of overlapping communities, and whose tools are “macroscopic”: statistics, epidemiology, and policy.
Bench science and public health are two concepts that don’t often appear in the same sentence. Practitioners of each have a different world view, literally and figuratively. When we picture a bench scientist, we imagine someone peering through a microscope, focused on the most minute components of health and disease. When we think of public health, we picture someone who sees the world as a series of overlapping communities, and whose tools are “macroscopic”: statistics, epidemiology, and policy.
However, “wet lab” or bench-trained scientists have always had a role in public health; they provide the insights into human and cellular biology that underwrite every aspect of society’s understanding of the causes and control of disease. In addition, especially in recent years, bench-derived cellular and molecular techniques have been adapted to play a role in public health investigations.
Molecular epidemiology, as best demonstrated by tuberculosis outbreak analysis[1] and foodborne disease surveillance systems such as PulseNet[2], has remade our understanding of communicable disease transmission and immunology, to say nothing of public health control efforts. “Fingerprinting” an organism—whether by pulsed field gel electrophoresis or by DNA sequencing—allows epidemiologists to gain a far more nuanced understanding of outbreaks than microbial phenotypes ever did.
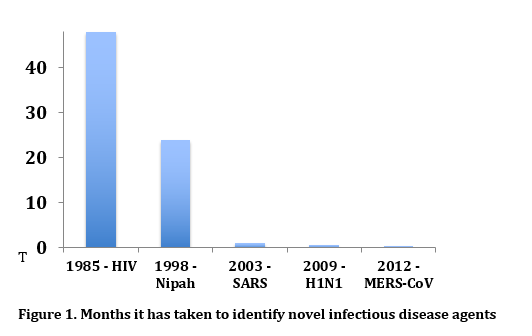
The time it takes to identify novel infectious disease agents, again using molecular genetic techniques, has decreased phenomenally in the last few decades, as shown in figure 1. The SARS-like virus, MERS-CoV, currently playing a lethal game of cat and mouse in the Middle East, was identified only days after its initial isolation in Saudi Arabia[3] compared to the four-plus years that it took to identify HIV.
Public health bench researchers, in response to novel infectious disease outbreaks, create “home brew” molecular diagnostic tests months and sometimes years before commercial tests are available. Given the pace at which infections can spread around the world, public health scientists don’t have time to wait for the validation and testing process necessary for FDA approval to release a test for widespread use.
Genomics is another area that is remaking our understanding of population biology and epidemiology. It took three years and $10,000,000, from 2001 to 2004, to go from a first draft to a final complete sequence of the human genome. Now sequencing an entire human genome can be done in less than a day for $1,000. Tens of thousands of prokaryotic and eukaryotic genomes have been sequenced, many with an eye toward understanding the diseases encoded in their genetic material. Sequencing a portion of the genome of cholera isolates in Haiti allowed rapid determination of the South Asian origin of the strain[4]. Knowledge of influenza genetic variation based on sequencing allows public health officials to predict the distribution and evolution of new strains and antimicrobial resistance[5].
Genome-wide association studies (GWAS) are pursuing the genetic risk factors for cardiovascular disease, cancer, and diabetes. The Framingham Heart Study, profiled elsewhere in this issue, was one of the first population-based studies to apply GWAS to its traditional epidemiologic data[6]. Using “paleogenetics,” sequence data for H. pylori have been analyzed to understand the pattern of original human migration in the Pacific region, and to infer the social, dietary, and disease interactions in human populations[7].
The ability to control HIV or cancer will not come from an observational study but from the bench. Epidemiology may help the bench researcher focus his or her efforts, and ultimately, public health will roll out the vaccinations and cures that bench scientists discover. It’s this give-and-take between basic and population science that advances human knowledge and human health.
References
- Lawn SD, Zumla AI. Lancet, 2011.
- Jones TF, et al. Foodborne Pathog Dis, 2007.
- Zaki AM, et al. NEJM, 2012.
- Chin CS, et al. NEJM, 2011.
- Whitley RJ, et al. Clin Infect Dis, 2013.
- Ehret GB. Glob Heart, 2013.
- Falush D, et al. Science, 2003; Moodley Y, et al. Science, 2009.
About the Author
Dr. Rebecca Wurtz is the MPH program director at Northwestern University and an Associate Professor in Preventative Medicine. She was previously the Deputy Medical Director of the Illinois Department of Public Health and the President of the Chicago Board of Health.
Two years into the HIV epidemic, Dr. Rebecca Wurtz attended a talk given by a CDC epidemiologist who declared definitively that an infectious disease was the cause of the mysterious and deadly immunologic illness, ending speculation that Gay-Related Immunodeficiency was caused by a recreational drug or a toxin. It would be another two years before the causative virus was identified. As the pace of spread of infectious diseases has quickened, so has the pace of scientific discovery into their causes and control. Here Dr. Wurtz writes about the hand-in-hand relationship of basic science and public health.
