by mjb843 | Feb 28, 2016 | Fundraisers, GlobeMed
On November 17-20 the GlobeMed Campaigns Team put on the annual Sweater Sale. Here is Jason Chen, Co-President of Campaigns, on the fundraiser in review. I believe that the annual fall ugly sweater sale is consistently our most successful fundraiser. We large amount...
by mjb843 | Feb 16, 2016 | Social Justice
By Elizabeth Kim Religion is not the first thing that comes to mind in college classrooms, let alone the field of global health. Mention of religion in the media and in the current presidential elections have forced it to have a negative connotation. However,...
by mjb843 | Feb 10, 2016 | Uncategorized
By John Galyas Before I stepped foot on campus to begin my freshman year at Northwestern, I knew I wanted to join GlobeMed. I had spent the last few weeks of the long summer before my freshman year Googling anything and everything about Northwestern in an admittedly...
by mjb843 | Feb 4, 2016 | GlobeMed, Social Justice
“Instead of treating social justice issues as trendy news topics or points of discussion, we should acknowledge that all social justice issues deserve to be recognized and fought for.” My name’s Camille Cooley. I’m a sophomore in SESP studying...
by mjb843 | Jan 26, 2016 | Uncategorized
By Tamar Eisen The most common question I have heard after returning to Northwestern for winter quarter is, “How was the world?” The reason I am consistently asked this question is because last fall, I went on a semester-long comparative health program to India, South...
by mjb843 | May 12, 2015 | globalhealthU, Uncategorized
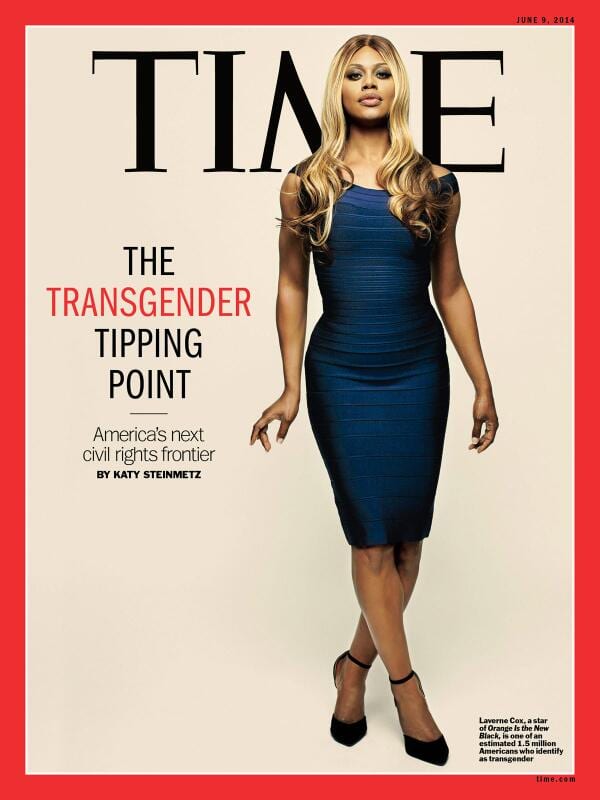
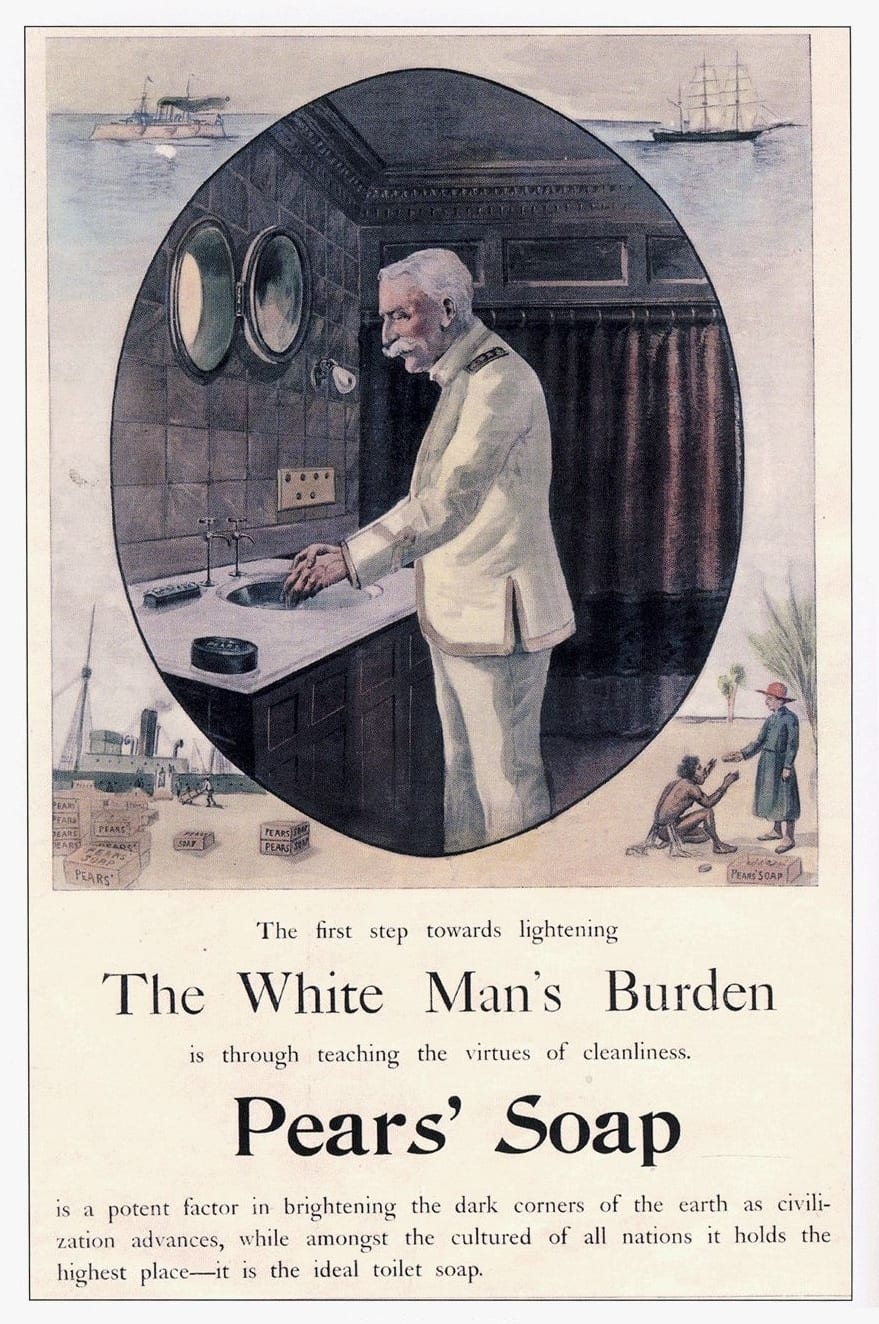
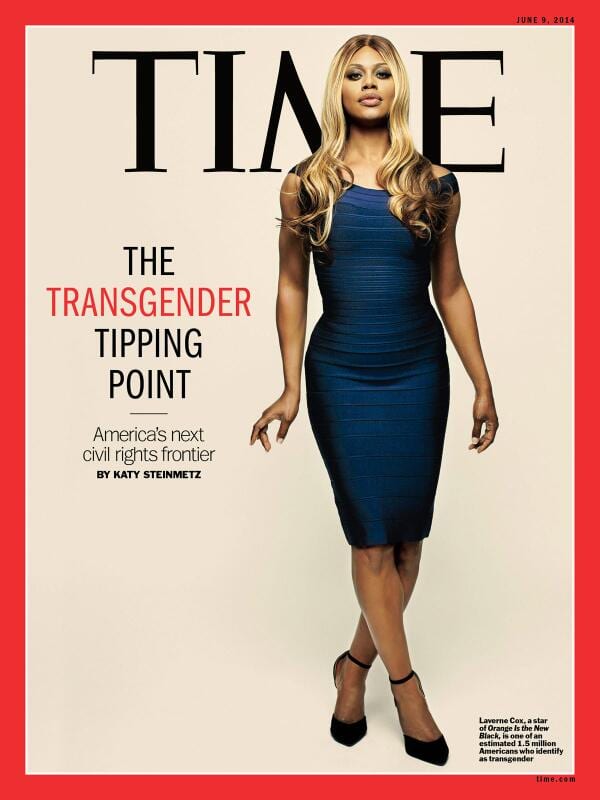
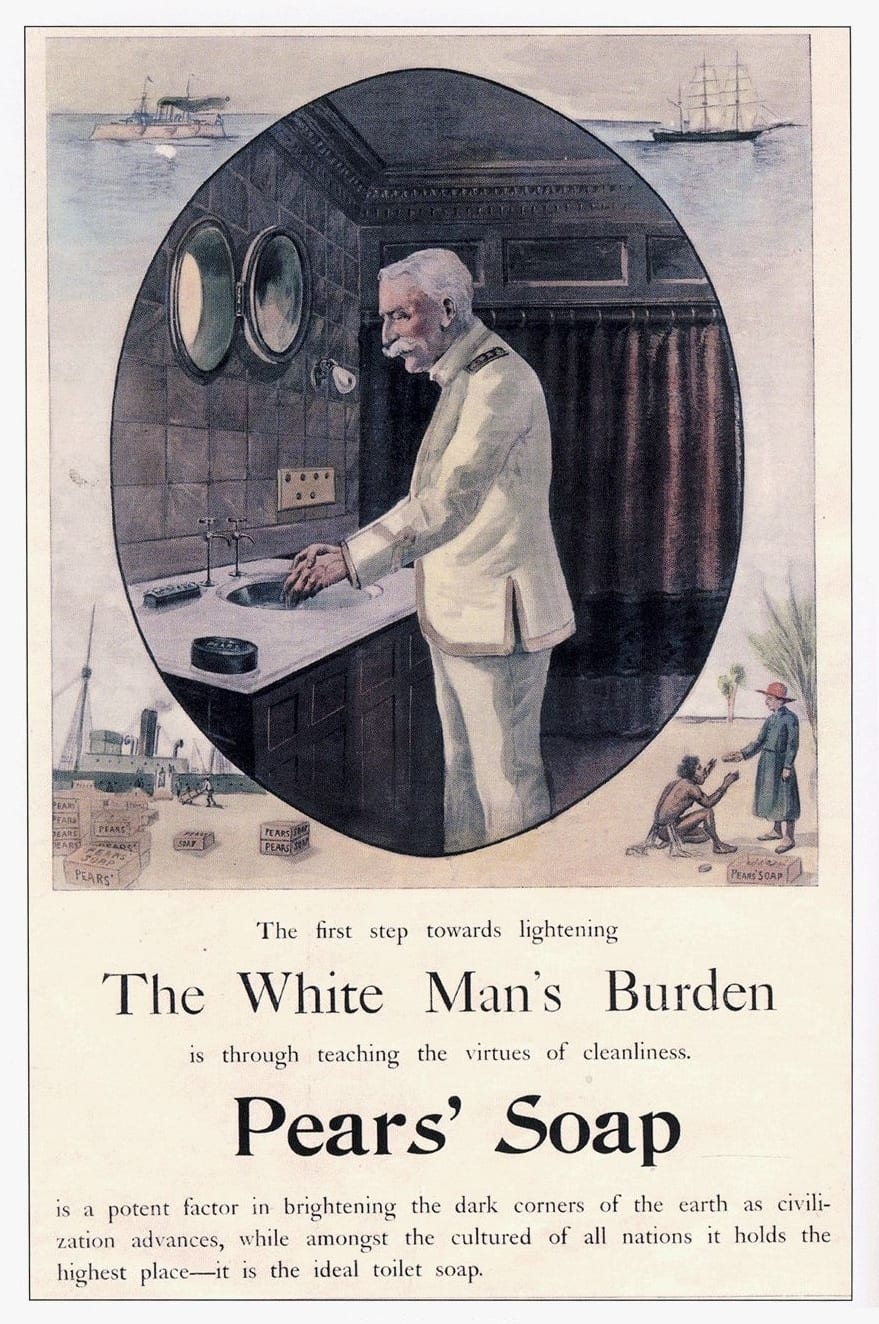
By Amy Lin Last quarter, the ghU sessions delved into the topics of gender and sexuality. While the sessions were empowering and fun as a woman, it was easy to get swept up in the feminist movement and start saying things like “gender is a social construct” and “down...
by mjb843 | Mar 2, 2015 | Uncategorized
By Elizabeth Kim This winter quarter’s GHUs at GlobeMed Northwestern has focused on gender and sexuality, of which transgender has been a topic of discussion. The overwhelming consensus in the discussions and in US classrooms is that there is not enough education...
by mjb843 | Feb 18, 2015 | Global Health, Social Justice, Uncategorized
By Nida Bajwa Anyone who has studied global health knows that the field is wrought by many many failures, and very few successes. It is easy to get discouraged from the field when analyzing the immense amount of failure and repetition of those failures in the field....

by mjb843 | Feb 9, 2015 | Global Health, Policy, Uncategorized
By Gordon Younkin You may have seen in the news a little over a year ago that the WHO declared Nigeria free of guinea-worm disease. While this may be considered old news, it is still worth examining the campaign that successfully stopped its transmission. Guinea-worm...

by mjb843 | Jan 26, 2015 | Uncategorized
By Alissa Zhu With more than 50 chapters spread across colleges and universities across North America, it’s hard to imagine less than a decade ago, GlobeMed was only an idea in Victor Roy’s head. GlobeMed co-founder Victor Roy Skyped in from the United Kingdom Sunday...